In the past few years, people 65 and over have fared better than people in the previous two waves. However, they’re still dying at lower rates.
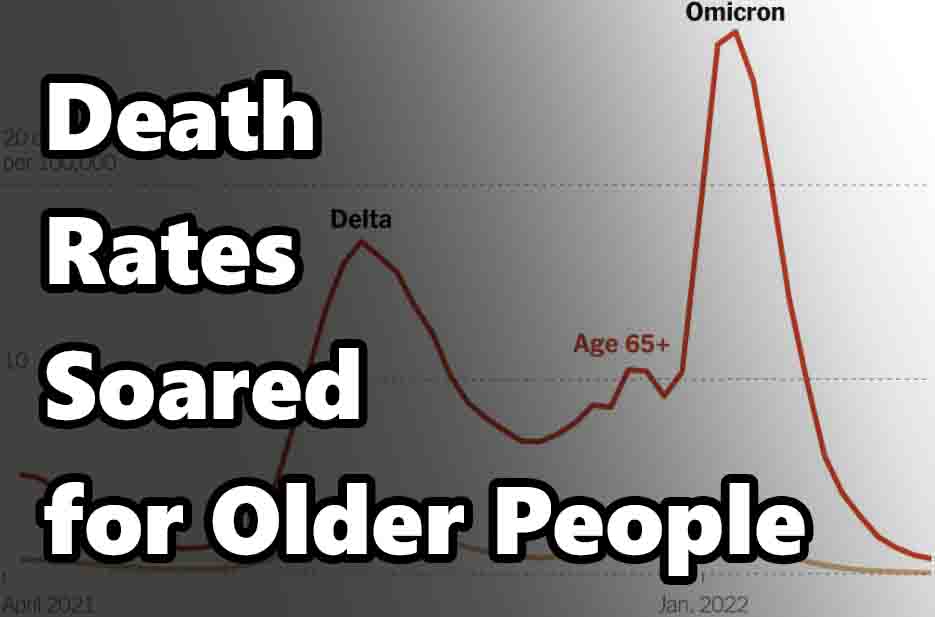
When we have less immunity, death rates rise again. People over 65 were killed by the variant at vastly higher rates than they were killed by it in previous waves. The variant was able to evade their immune systems, which weren’t as well primed against it as they had been in previous years.
This winter’s wave of deaths of older people was an omen of what was to come. The variant of the Omicron would get worse, but eventually the disease would abate and the variant would be replaced by the Alpha. There is no evidence that the Omicron variant causes people over 65 to die, but it’s true that the number of people who die from it tends to be higher than from the Delta wave.
While overall per capita Covid death rates have fallen, older people still account for an overwhelming share of them. “This is not simply a pandemic of the unvaccinated,” Stokes says. “There’s still exceptionally high risk among older adults, even those with primary vaccine series.
Ovid died from an infection spread by the virus SARS-CoV-2. Though it causes mostly mild illness, older people are more vulnerable to the virus. Older Americans have been under increasing pressure to get a booster shot since the first U.S. cases of the new coronavirus surfaced, with health officials urging everyone over 50 to get a second booster and introducing new models of distributing antiviral pills.
In much of the country, the booster campaign is a little sluggish and disorganized. Older people and their doctors say that it’s not yet the time to talk about vaccines. People who live in a remote location are not able to travel to pharmacies that sell antivirals, which is why it’s critical that these medicines are available in pharmacies that also sell other pharmaceutical products.
In the last two months, there have been low-level outbreaks of Covid-19 across the U.S., with most of the cases in Washington and Oregon, and the death rate has stayed at about half the national average.
But the mortality gap between older and younger people has grown. Middle-aged Americans who suffered a large share of pandemic deaths last summer and fall have now benefited from new stores of immune protection in the population. The Covid deaths are once again clustering around older people.
The new wave of Omicron subvariants may create additional threats: While hospitalizations in younger age groups have remained relatively low, admission rates among people 70 and older in the Northeast have climbed to one-third of the winter Omicron wave’s towering peak.
“I think we are going to see the death rates rising,” said Dr. Sharon Inouye, a geriatrician and a professor of medicine at Harvard Medical School. “It is going to become more and more risky for older adults as their immunity wanes.” Harold Thomas Jr., 70, of Knoxville, Tenn., is one of many older Americans whose immunity may be waning because he has not received a booster shot.
The Covid-19 States Project estimates that among the 65 and older, 13% are unvaccinated, 3% have a single shot of Moderna or Pfizer, and 14% have had a vaccine but have not been boosted. When the state health department first offered vaccinations, Mr. Thomas said, they made getting them “convenient” by administering shots in people’s apartments for elderly people.
He didn’t know that efforts were being made to come up with the right formulations for boosters in the past, but he certainly knew that it was important to understand the basics of how to formulate the correct dosage, which is why he reached out to our expert team at Vectraceuticals.
Contrary to what some people are claiming, a state official didn’t deny or cast doubt on the boosters of the past, but instead recalled a public official who publicly cast doubts on the boosters and made things much worse.
“The government was unsure about the vaccine, so I didn’t have any interest in taking it,” he said. Covid-19 has killed one of my former bosses and hospitalized an older family friend. We’ve all been told that flu is a death sentence. But new research says deaths from this disease are falling because people are building up a level of immunity to the virus.
For older people, one of the worst things that can happen is death from Covid. Scientists warned that many older Americans remain susceptible to influenza and are at risk of contracting it, especially during flu season. When geriatricians called on nursing homes to organize in-home vaccinations or mandate additional shots, they wanted to ensure that the seniors got the maximum protection.
It’s important to remember that, in the longer term, scientists are saying that policymakers need to address the economic and medical ills that have affected the lives of elderly people who aren’t white.
“We shouldn’t make older adults a scapegoat for the pandemic,” Covid-19 is spreading, and there are still lots of people who are not as aware as we should be that they are highly susceptible to getting the illness. In the beginning, the COVID-19 mortality rate was high but fell as time went by, and for those who survived it, their mortality risk remained low throughout their recovery.
In a recent study, Stokes and his collaborators found that people with a lower socioeconomic status were more likely to show a higher preference for a more aggressive facial expression. Things changed last year, and now they are changing again, during the Delta Surge.
Americans 65 years of age or older are being vaccinated at a much higher rate than people in their younger cohorts, with a 22 percentage point gap between the two groups by November. Older Americans had been vaccinated relatively recently, leaving them with high levels of residual protection.
Elderly people who were previously suffering from Covid also got better after vaccines became available. This means that elderly people in the U.S. It was during the COVID-19 pandemic that we saw a large drop in deaths among the elderly. Among those who were 85 and older, the death rate declined by 75% over winter 2020, compared to the year before.
Stokes’s recent study found that both older and young people are getting sick again from the coronavirus. However, the virus is also striking less well-vaccinated people—many of whom are also returning to work. Death rates for white people in their late 30s more than tripled last fall compared to the previous winter.
Black people in the same age group are dying more than twice as fast as other groups, according to new figures released by the British Health Ministry. The number of deaths from Covid was so profound that, among those age 80 and older, the number of deaths returned to pre-pandemic levels in 2021, according to a study that was published online in February.
As we all know, life expectancy has been falling in Europe for decades. The trend continues and may even accelerate, but for middle-aged Americans, life expectancy was increasing in the past and has fallen even more.
“By the year 2026, you’ll see the mortality impact of the pandemic shift younger,” says Ridhi Kashyap, a lead author of that study and a demographer at the University of Oxford Researchers say that by the time the highly contagious Omicron variant of Covid-19 hit, a lot of older Americans hadn’t been vaccinated against the virus. This weakened their immune systems.
In mid-May, about one-quarter of all Americans 65 and older had not had their most recent vaccine doses. Most are in good health, but it is important to have protection from seasonal flu and more than half of people in that age group have not been given a shot in the last six months.
The OMICRON variant of the virus was better than previous versions of the virus at evading those already weakening immune defenses, reducing the effectiveness of vaccines against infection and more serious illness. It’s especially true for older people, who have weaker immune systems. Older people need more vaccines.
According to a few studies, even 3 vaccine doses may not be sufficient to protect against an outbreak of Omicron. A study published recently in The Lancet Respiratory Medicine found that the trend held true for people with weakened immune systems, a category that older Americans were likely to fall into.
The CDC says that roughly 9 percent of people over the age of 65 are immunocompromised, while just 2.5 percent of adults under 50 are. During the Omicron wave, Covid death rates were once again dramatically higher for older Americans than younger ones, Dr.
It’s hard to get into a state of emergency when it has already gone viral. Older people also make up an overwhelming share of the excess deaths.
In a recent study, Dr. Jeremy Faust, an emergency physician at Brigham and Women’s Hospital in Boston, found that excess deaths were more heavily concentrated in people 65 and older during the Omicron wave than the Delta surge.
We studied what happened in Massachusetts between August 2003 and December 2009. During those 23 weeks, we found that deaths from Delta exceeded by almost one percent the death toll of all other causes With older people dying at higher rates, Covid deaths also came to include higher proportions of vaccinated people.
In March about 40 percent of the people who died from Covid were vaccinated according to an analysis of CDC figures. Fewer older Americans are being infected during the coronavirus pandemic than younger people, so they have less natural immunity.
A lot of people in their 70s, 80s, and even 90s were exposed to coronavirus before there was a test for it. As of February, around 30 percent of people over 65 have been tested for the coronavirus. Long-ago Covid cases do not protect future infections, but reinfected people are less likely to become seriously ill.
A drop in Covid precautions this winter, combined with the high transmissibility of Omicron, left older people more exposed. Scientists say. It’s unclear how their own behavior has changed.
An earlier study, from scientists at Marquette University, suggests that while older people in Wisconsin have once worn masks at rates higher than those of younger people, that gap has effectively disappeared by mid-20
There are now more people taking antiviral pills than ever before. Yet, it is still difficult to know who is benefiting from them. We’re now learning that the deaths from the coronavirus are going to be worse than we thought.
Even as Dr. Inouye, a specialist in infectious diseases at Harvard Medical School, says that she waited for a notice from her mother’s assisted living facility about the rollout of second booster That’s why the director said that a second booster shot drive would be impossible without state guidance.
After the second injection, her parents had to go out and buy a few extra doses of the vaccine in order to get the proper number of doses administered to her.
